Document Type : Original Article
Authors
1 DVSc Candidate, Department of Internal Medicine and Clinical Pathology, Faculty of Veterinary Medicine, Urmia University, Urmia, Iran
2 Department of Internal Medicine and Clinical Pathology, Faculty of Veterinary Medicine, Urmia University, Urmia, Iran
Abstract
Displacement of the abomasum is a common disease of the gastrointestinal tract in dairy cattle. Abomasal displacement has been associated with abomasal hypomotility. Therefore, it is necessary to identify effective therapeutic agents that stimulate abomasal motility in cattle. Yarrow (Achillea millefolium) is traditionally used as a folk remedy for treatment of human gastrointestinal complaints in the northwest of Iran. This study investigated the effects of A. millefolium extracts on abomasal smooth muscle preparations from healthy cattle. The A. millefolium extracts (3 to3000 mg L-1) contracted the isolated of smooth muscle in a concentration-dependent manner, with an effective threshold concentration of 30 mg L-1 (p < 0.05). The strongest contraction by A. millefolium aqueous extracts in a concentration of 3000 mg L-1 was observed and amounted to 124.90 ± 10.80% of the control treatment. This action was unaffected by pretreatment with hexamethonium and indomethacin, but strongly reduced by verapamil, atropine and 4-DAMP. The inhibiting effect of 4-DAMP and atropine suggesting that the effect of A. millefolium extracts is mediated at least partly by M3 muscarinic acetylcholine receptor. The results suggested that A. millefolium has the potential prokinetic effect that may prevent or alleviate dysfunctions of gastrointestinal motility.
Keywords
Main Subjects
Introduction
Impaired abomasal motility is common in dairy cattle and is suspected to play a major role in the occurrence of left displaced abomasum, abomasal volvulus and abomasal impaction in cattle.1,2 Abomasal motility decreases in many ailments, namely ketosis, hypocalcemia, hyperinsulinemia, and reduced insulin sensitivity that have been studied and reported in recent publications.3-7 Thus, it would be clinically helpful to identify effective prokinetic drugs that stimulate, coordinate and restore abomasal motility in cattle.
The importance of the parasympathetic nervous system in the physiology of GI motility and in the pathophysiology of motility disorders has been described in cattle.8 In the cholinergic system, the main endogenous neurotransmitter, acetylcholine (ACh), activates G-protein coupled muscarinic receptors. Smooth muscle contraction in GI organs is the most important effect of the activation of muscarinic receptors located directly on smooth muscle cells or on the nerve cells of the GI nervous system.9
Several investigations have been carried out in characterizing muscarinic receptors in the digestive tract of cattle. In the bovine gut smooth muscle, it has been shown that mRNA transcripts and binding sites of M2 and M3 AChR subtypes are the most abundant with a ratio of 5:1.10 In the clinical setting, left-side displacement of the abomasum (LDA) in cows did not alter the extracellular components of M2 and M3 receptors in the GI tract, whereas receptor densities were lower in the intestinal wall (mainly duodenum) of cows with LDA.8
Bethanechol, a well-known prokinetic drug, induces contraction of smooth muscle cells by direct stimulation of muscarinic receptors. In vitro studies on smooth muscle preparations revealed a bethanechol-induced, contractility in muscle strips from the esophageal groove of calves11 and the abomasum of healthy cows.12 However, chemical drugs often have limitations such as serious adverse side effects.9
Therefore, herbal products may be an attractive alternative thanks to their lower risk their proved prokinetic effects.13-15 Achillea millefolium L. (Yarrow) which belongs to the Asteraceae family is one of the most widely used medicinal plants in the world.16
In West Azerbaijan (Iran) the aerial parts of the plant have been used traditionally to treat gastritis, cancer, hemorrhoids, vertigos, anemia, anorexia, dyspepsia, gastralgia, hemorrhage, dysmenorrhea and diarrhea.17
Preclinical studies indicate that yarrow may have anti-inflammatory, hepatoprotective, antinociceptive, anxiolytic and antimicrobial activities. Animal studies have also shown that it is generally safe and well tolerated.16
In Italy leaves of yarrow are used to make an ointment cooking them over a low heat with olive oil, talon, bee’s wax and egg yolk; this is applied locally to cure sores on bovines’ withers caused by yoke rubbing.18 In British Columbia, Canada, the extract of plant flowers has been used to treat diarrhea and gastritis in dogs and cats. It is given orally with a syringe or put in the drinking water.19
The main constituents of yarrow are volatile oils (sabinene, β-pinene, 1,8-cineole, artemisia ketone, linalool, α-thujone, β-thujone, camphor, borneol, fenchyl acetate, bornyl acetate, (E)-beta-caryophyllene, germacrene D, caryophyllene oxide, beta-bisabolol, delta-cadinol, chamazulene); flavonoids (apigenin- and luteolin-7-glycosides, and rutin); and alkaloids.20
In the current study, we used extracts of yarrow to assess its reported prokinetic action on smooth muscles in the rodent and human gastrointestinal tract,21 to investigate their regulatory effects on contractions of the smooth muscles of the bovine abomasum, and also elucidate its mechanism of action.
Materials and Methods
Chemicals. Acetylcholine chloride (ACh), atropine sulfate, hexamethonium, indomethacin, verapamil hydrochloride and 4-DAMP were purchased from Sigma Chemicals Co. (St Louis, USA). Calcium chloride, potassium chloride, sodium chloride, glucose, magnesium sulfate, potassium dihydrogen phosphate, sodium bicarbonate, ethanol and chloroform were obtained from Merck (Darmstadt, Germany).
Plant material and extraction. Aerial parts of A. millefolium were collected from the northwest of Iran in 2015. The plant was identified in the Department of Botany, Tarbiat Modarres University of Tehran, Tehran, Iran and a sample was deposited in the herbarium of the Department of Medicinal and Industrial Plants, Urmia University, with the voucher number of 5374. The plant material was cleaned, shade-dried and coarsely grounded. The powdered material was extracted with 70% ethanol by cold maceration for three days with occasional shaking. It was filtered through a muslin cloth and then through a Whatman qualitative grade 1 filter paper (Sigma).
This procedure was repeated twice and the combined filtrate was evaporated in a rotary evaporator to obtain hydroalcoholic extract of A. millefolium. A part of this extract was used in the pharmacological studies and the other part was used for the fractionation. The extract was suspended in distilled water and extracted with chloroform. The mixture was allowed to separate into two layers. The upper layer (aqueous fraction) was again taken into a separating funnel; ethyl acetate was added to it, separated and evaporated with the rotary evaporator to get the ethyl acetate fraction. The remaining lower layer was collected and evaporated to obtain the A. millefolium aqueous extract (AMAE).
Preparation of smooth muscle and data acquisition. Tissue samples were collected from routinely slaughtered Holstein crossbred dairy cows (4 to 8 years old; n = 18) with no previous history of abomasal displacement or other abomasal disorders. The abomasum was removed within 20 min after stunning. Full-thickness specimens were harvested from the body of the abomasum by dissecting a rectangular piece of tissue (6 × 15 cm) from the location. Tissue specimens were immediately rinsed with cooled (4 ˚C) Krebs solution (composition (mM): NaCl, 118.00; KCl, 4.75; MgSO4, 1.20; KH2PO4, 1.20; CaCl2, 2.50; NaHCO2, 25.00 and glucose, 11.50).
Specimens were stored in 1 L of cooled (4 ˚C) Krebs solution that had been oxygenated (95% O2 and 5% CO2) for 1 hr; and were transported from the slaughterhouse to the laboratory within 15 min. The whole pieces of tissue were placed in a petri dish filled with Krebs solution at room temperature and the mucosa was carefully removed from the muscle layers, and tissue strips (15 × 2 mm) were cut from the abomasal body muscle fibers.
The abomasal strips were mounted in separated 25 mL chambers, maintained at 37 ˚C in Krebs solution, and gassed continuously with a mixture of 95% O2 and 5% CO2. One end of each strip was fixed to the bottom of the chamber, and the other end was attached to an isometric muscle transducer (model TRI 202P; PanLab, Barcelona, Spain) coupled to bridge amplifier (model ML224; AD Instruments, Castle Hill, Australia) and data acquisition PowerLab system (model ML870; AD Instruments) using Labchart software (version 8.0, AD instruments).
Specimens were allowed to equilibrate in the organ bath for 1 hr, whereby muscle tension was preset to 2 g in two steps (1 g each) at 10 min intervals and during this time Krebs solution was replaced every 15 min with fresh solution. All specimens were tested for functional viability prior to and after all experiments by the addition of 1 mM acetylcholine to the organ bath. The dose-response curves to determine the effect of acetylcholine were obtained by exposing the preparation to increasing concentrations added to the bath (2 min to each concentration).
Then the submaximal (inducing responses approximately 70% of the maximum) concentration was determined for each of the strips. Strips producing three consistent repeatable responses to submaximal concentration of acetylcholine were used.
After removal of acetylcholine through wash out, the abomasum responses were observed in the presence of increasing cumulative concentrations of A. millefolium aqueous and hydroalcoholic extracts (3 to 3000 mg L-1).
To assess the possible mechanisms underlying the contractile effect of the aqueous fraction on abomasal strips, atropine, a muscarinic receptor blocker (10 µM); hexamethonium, a nicotinic nACh (NN) receptor anta-gonist (10 µM); indomethacin, a prostaglandin synthesis inhibitor (10 µM); and 4-DAMP, a muscarinic M3 receptor antagonist (10 µM) and verapamil, a calcium channel blocker (0.1 µM) was added to the organ bath 10 min prior to the addition of the extract (3 to 3000 mg L-1).
Statistical analysis. Data were examined graphically for assumptions of normal distribution and homogeneity of variation. Nonparametric statistical test was used for analysis because the assumptions were not met normal distribution. The Friedman repeated measures analysis of variance on ranks was used to compare results in strength of contractions between different concentrations of the extract. Overall p < 0.05 was considered significant.
Pair-wise comparisons between each treatment group (concentration) versus control group were made using Dunnett's Method.
Results are expressed as medians and interquartile ranges (25th - 75th percentiles). Data were analyzed using SigmaPlot for windows (version 12.3; Systat Software, Inc. San Jose, USA).
Results
We tested 72 specimens by the use of Acetylcholine chloride to determine functional viability and only six specimens did not respond to stimulation with Acetylcholine chloride. All 66 specimens tested at the end of the recording period had the expected response to Acetylcholine chloride and showing that the muscle was not damaged by non-specific action.
Acetylcholine (1 to 10 µM) caused a concentration-dependent contraction of the cattle abomasum.
The solvent as a control (distilled water), did not exert an effect on basal tonus of any preparations of cattle abomasum.
The A. millefolium aqueous and hydroalcoholic extracts (3 to 3000 mg L-1) contracted the isolated strips of cattle abomasum smooth muscle in a concentration-dependent manner, with an effective threshold concentration of 30 mg L-1 (p < 0.05, Fig. 1) but treatment of tissue strips with 3 and 10 mg L-1 of A. millefolium extracts did not show any significant difference with the control. A typical trace, showing the effect of the A. millefolium aqueous extract (3 to 3000 mg L-1) is covered in Figure 2A.
When the organ bath was drained and Krebs was added, there was a rapid relaxation of the muscle to baseline of resting tension. Atropine at 10 µM, concentration did not affect the spontaneous smooth muscle contractions but abolished the contractile effect of Ach. Treatment of the tissues with atropine (10 µM) completely abolished AMAE induced smooth muscle contractions (Fig. 2B). Furthermore, the M3 muscarinic receptor antagonist 4-DAMP (10 µM) revealed an inhibition of contractions caused by AMAE (Fig. 2C), while either hexamethonium (10 µM) or indomethacin (10 µM) had no impact (data not shown).
Verapamil at the bath concentration of 0.1 µM dramatically inhibited the contractile amplitude and tension induced by AMAE (Fig. 2D).
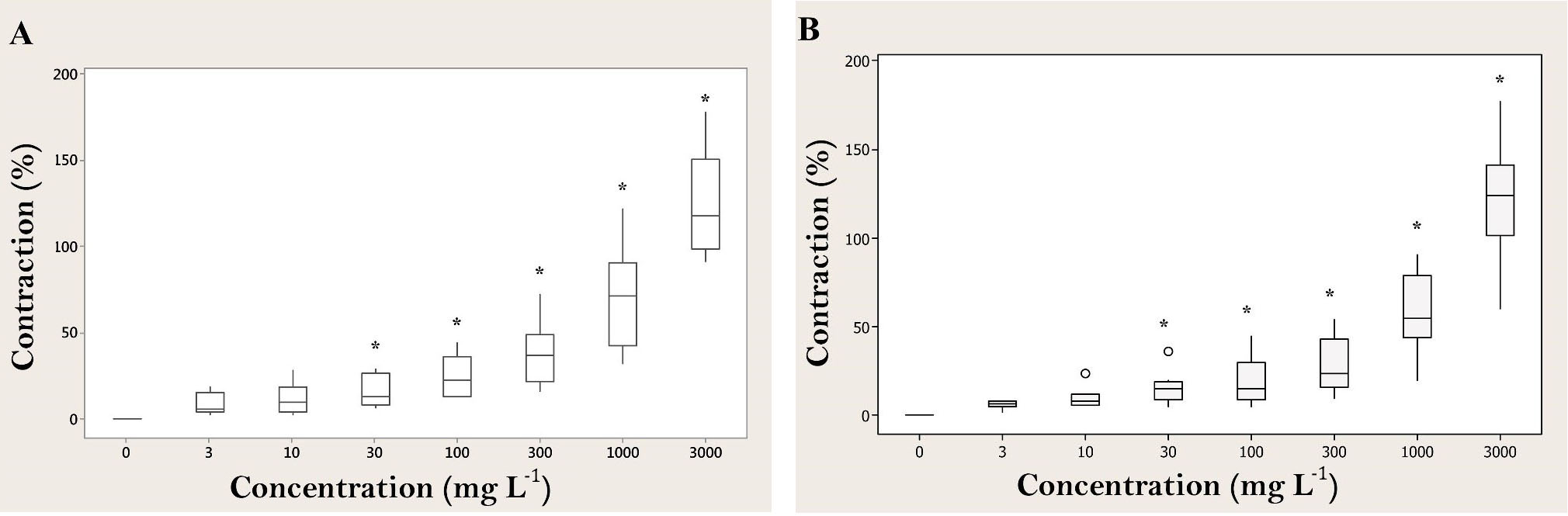
Fig. 1. Box plots for effects of A. millefolium aqueous extract (n = 8) (A) and hydroalcoholic extract (n = 8) (B) on basal tonus of healthy cattle abomasal preparations. Each box represents the central 50% of the values, the horizontal line within each box represents the median value, and the whiskers indicate the range of values that are within the inner boundary. Values outside the inner fence are plotted as empty circles (o). ٭ indicates significant differences compared to control (p < 0.05).

Fig. 2. Basal contractions and dose dependent response of abomasal smooth muscle to AMAE (A). Inhibitory effects of atropine (B), 4-DAMP (C), and verapamil (D) on the AMAE-induced contractions of abomasal smooth muscle.
Discussion
The main findings of this study were that the A. millefolium extracts induced a significant increase in contractility of smooth muscle preparations of abomasum. The spasmogenic effect of aqueous extract was completely abolished in the tissues pretreated with atropine, similar to that of ACh. Results of this study confirmed the presence of cholinergic constituent(s) in the extract of the plant responsible for the spasmogenic response. Acetylcholine ,a neurotransmitter of the parasympathetic nervous system, has an important role in abomasal motility,22 and its action is mediated by the activation of muscarinic receptors, whereas atropine is a muscarinic receptor blocker.12
Our findings were in agreement with a previous study that demonstrated the aqueous extract of dried flower heads of yarrow exerted a direct spasmogenic effect on mouse and human gastric antrum.21
When the stimulant effect of AMAE was studied in the presence of hexamethonium, a ganglion blocker or indomethacin, a prostaglandin synthesis inhibitor, it remained unchanged, suggesting the presence of ACh-like constituents independent of nicotine receptors activation or prostaglandin synthesis inhibition.
Acetylcholine, the main endogenous neurotransmitter in the cholinergic system, causes a contraction of the smooth muscle layers in the forestomach and abomasum through activation of muscarinic receptors8,23 located directly on smooth muscle cells or nerve cells of enteric nervous system.24 It has been demonstrated that M3 mAChRs play a predominant role in the mediation of contraction in smooth muscle preparations, even though M2 mAChRs were detected at higher density than M3 mAChRs.25,26
Regarding in these information, we examined whether AMAE-induced contraction was mediated, at least, by activation of the M3 muscarinic receptors and observed that the muscarinic M3 receptor-preferring antagonist, 4-DAMP, completely blocked the AMAE-induced contractions.
Although it has been suggested that the extent of contribution of the muscarinic M3 receptors differs with the type of smooth muscles and the species of animals,27 we consider that AMAE may have high affinity with the muscarinic M3 receptors, Accordingly the contractile response of the abomasal smooth muscle to AMAE may chiefly result from the activation of muscarinic M3 receptors. However, to clearly understand these speculations, further studies are needed to elucidate the pharmacological affinity of AMAE with the muscarinic receptor subtypes.
Pretreatment of tissues with verapamil, a standard calcium channel blocker, inhibited muscle contractions induced by AMAE, confirming the action of extract on abomasal motility was medicated by Ca2+ influx. The M3 muscarinic receptor is coupled to Gq-type G proteins, resulting in the activation of the second messengers inositol trisphosphate which induces Ca2+ release from intracellular Ca2+.28
In smooth muscle cells, increase in cytoplasmic calcium concentration is the primary stimulus for contraction, which is generally the result of both release of intracellular stored calcium and the influx of extracellular calcium.29
The main pathway for Ca2+ entry into intestinal smooth muscle cells is through L-type Ca2+ channels. Verapamil is a calcium channel blocker that has been used to promote the relaxation of smooth muscle cells by inhibiting calcium influx through calcium channels and calcium release from intracellular stores.30,31
In a previous study, the chemical composition of yarrow has been analyzed in detail and extracts of this plant have been demonstrated to contain a number of pharmacological active ingredients, including alkaloids such as choline and flavonoids such as rutin and apigenin.21 Borrelli et al. also indicated that choline, is the chemical ingredient of yarrow responsible for the gastric contractile effect. Further studies are warranted to investigate the in vivo effects of AMAE in animals suffering from LDA.
Acknowledgements
This study was supported by the Faculty of Veterinary Medicine, Urmia University. The authors would like to thank Dr. Amin Mamaghani for his valuable contributions.
- Doll K, Sickinger M, Seeger T. New aspects in the pathogenesis of abomasal displacement. Vet J 2009;181:90-96.
- Ozturk AS, Guzel M, Askar TK, et al. Evaluation of the hormones responsible for the gastrointestinal motility in cattle with displacement of the abomasum; ghrelin, motilin and gastrin. Vet Rec 2013;172:636.
- Chapinal N, Carson M, Duffield TF, et al. The association of serum metabolites with clinical disease during the transition period. J Dairy Sci 2011;94:4897-4903.
- Mokhber Dezfouli M, Eftekhari Z, Sadeghian S, et al. Evaluation of hematological and biochemical profiles in dairy cows with left displacement of the abomasum. Comp Clin Pathol 2013;22:175-179.
- Mercadante PM, Ribeiro ES, Risco C, et al. Associations between pregnancy-associated glycoproteins and pregnancy outcomes, milk yield, parity, and clinical diseases in high-producing dairy cows. J Dairy Sci 2016;99:3031-3040.
- Suthar VS, Canelas-Raposo J, Deniz A, et al. Prevalence of subclinical ketosis and relationships with postpartum diseases in European dairy cows. J Dairy Sci 2013;96:2925-2938.
- Dhakal K, Tiezzi F, Clay JS, Maltecca C. Inferring causal relationships between reproductive and metabolic health disorders and production traits in first-lactation US Holsteins using recursive models. J Dairy Sci 2015;98:2713-2726.
- Ontsouka EC, Niederberger M, Steiner A, et al. Binding sites of muscarinic and adrenergic receptors in gastro-intestinal tissues of dairy cows suffering from left dis-placement of the abomasum. Vet J 2010; 186:328-337.
- Steiner A. Modifiers of gastrointestinal motility of cattle. Vet Clin North Am Food Anim Pract 2003; 19:647-660.
- Stoffel MH, Monnard CW, Steiner A, et al. Distribution of muscarinic receptor subtypes and interstitial cells of Cajal in the gastrointestinal tract of healthy dairy cows. Am J Vet Res 2006;67:1992-1997.
- Barahona MV, Sanchez-Fortun S, San Andres MD, et al. Acetylcholinesterase histochemistry and functional characterization of the muscarinic receptor mediating the contraction of the bovine oesophageal groove. J Auton Pharmacol 1997;17:77-86.
- Buehler M, Steiner A, Meylan M, et al. In vitro effects of bethanechol on smooth muscle preparations from abomasal fundus, corpus, and antrum of dairy cows. Res Vet Sci 2008;84:444-451.
- Nam Y, Lee JM, Wang Y, et al. The effect of Flos LoniceraeJaponicae extract on gastro-intestinal motility function. J Ethnopharmacol 2016;179:280-290.
- Brierley SM, Kelber O. Use of natural products in gastrointestinal therapies. Curr Opin Pharmacol 2011;11:604-611.
- Oka T, Okumi H, Nishida S, et al. Effects of Kampo on functional gastrointestinal disorders. Biopsychosoc Med 2014;8:5.
- Akram M. Minireview on Achillea millefolium Linn. J Membr Biol 2013;246:661-663.
- Miraldi E, Ferri S, Mostaghimi V. Botanical drugs and preparations in the traditional medicine of West Azerbaijan (Iran). J Ethnopharmacol 2001;75:77-87.
- Uncini Manganelli RE, Camangi F, Tomei PE. Curing animals with plants: traditional usage in Tuscany (Italy). J Ethnopharmacol 2001;78:171-191.
- Lans C, Turner N, Khan T, et al. Ethnoveterinary medicines used to treat endoparasites and stomach problems in pigs and pets in British Columbia, Canada. Veterinary parasitology 2007;148:325-340.
- Orav A, Arak E, Raal A. Phytochemical analysis of the essential oil of Achillea millefolium L. from various European Countries. Natural product research 2006;20:1082-1088.
- Borrelli F, Romano B, Fasolino I, et al. Prokinetic effect of a standardized yarrow (Achillea millefolium) extract and its constituent choline: studies in the mouse and human stomach. Neurogastroenterol Motil 2012;24: 164-171.
- Michel A, Mevissen M, Burkhardt HW, et al. In vitro effects of cisapride, metoclopramide and bethanechol on smooth muscle preparations from abomasal antrum and duodenum of dairy cows. J Vet Pharmacol Ther 2003;26:413-420.
- Poole DP, Littler RA, Smith BL, et al. Effects and mechanisms of action of the ergopeptides ergotamine and ergovaline and effects of peramine on reticulum motility of sheep. Am J Vet Res 2009;70:270-276.
- Ontsouka EC, Steiner A, Bruckmaier RM, et al. Quantitative mRNA analysis of muscarinic acetylcholine receptors in the intestine of dairy cows with spontaneous caecal dilatation-dislocation. Vet J 2009;180:259-261.
- Eglen RM. Muscarinic receptor subtype pharmacology and physiology. Prog Med Chem 2005;43:105-136.
- Ehlert F, Pak K, Griffin M. Muscarinic agonists and antagonists: effects on gastrointestinal function. In: Fryer AD, Christopoulos A, Nathanson NM (Eds). Muscarinic Receptors. Berlin, Germany: Springer 2012:343-374.
- Barocelli E, Ballabeni V, Chiavarini M, et al. Regional differences in motor responsiveness to antimuscarinic drugs in rabbit isolated small and large intestine. Pharmacol Res 1995;31:43-48.
- Unno T, Matsuyama H, Sakamoto T, et al. M(2) and M(3) muscarinic receptor-mediated contractions in longitudinal smooth muscle of the ileum studied with receptor knockout mice. Br J Pharmacol 2005;146:98-108.
- Sanders KM, Koh SD, Ro S, et al. Regulation of gastrointestinal motility-insights from smooth muscle biology. Nat Rev Gastroenterol Hepatol 2012;9:633-645.
- Lyford GL, Farrugia G. Ion channels in gastrointestinal smooth muscle and interstitial cells of Cajal. Curr Opin Pharmacol 2003;3:583-587.
- Sanders KM, Kito Y, Hwang SJ, et al. Regulation of gastrointestinal smooth muscle function by interstitial cells. Physiology 2016;31:316-326.

